In addition to our own cookies, our website includes services from the following providers. All of these are strictly necessary to provide functionality to our site and may place their own cookies in your browser. Clicking ACCEPT ALL COOKIES indicates that you are also agree to cookies from the following providers:
Cloudflare
to display information that is relative to your geographical location, for example the correct course programme or application form. Without this service you might be looking at the wrong information for where you live.
Font Awesome
To create small icons to aid navigability. Without this service you might find it more difficult to navigate the site and it wouldn't look as nice.
Google Fonts and Icons
To allow us to use engaging text rather than boring old web fonts. Without this service you would be reading a less readable font.
Stripe
To allow us to take online payments. Without this service you might worry about the security of your payments, or whether they had been received.
Vimeo
To host any videos we include. Without this service, embedded videos might be slow to load and laggy to play.
Please click accept all to continue using our website.
Everything you need at one low price...
MRI in Practice Online
Everything you need at one low price
With the ever-rising cost of living and tight squeezes on training budgets, we strive to offer you the very highest quality MRI training and CPD fulfilment for a sensible, affordable, all-inclusive fee.
At £800 GBP ($1000 USD, A$1,600 AUD) our course price is the the most competitive it has ever been (adusting for inflation the course is now less than half the price it was in the year 2000).
Other providers charge high prices (per hour of taught content) seem to increase their prices every year and may even charge you numerous times for separate courses covering basics, advanced and clinical MRI. With our comprehensive programme you don't have to choose. When participants register on the MRI in Practice course, it includes all of the basics (including safety) plus the advanced topics and the clinical technique.
Our streaming lectures may be watched, rewound, and revised on demand and authors Dr Catherine Westbrook and Dr John Talbot, will be on hand to take any questions and provide any help or guidance on how to use our online learning environment.
If study leave is tight, or participants are very new to MRI, these sessions can be attended over two separate course deliveries if preferred. This allows participants to get a grasp of the basics and put them into practice before starting on the advanced subjects.

That's not all - the entire Handbook of MRI Technique course is included for free. Two courses for less than you would expect to pay for a single course!
Over the years, participants have often requested clinical technique sessions on the course. Time limitations of the live course made this impossible, now with our online format we can now include this content free of charge. We have created a separate course based on our Handbook of MRI Technique. After participants have enjoyed the 4-day MRI in Practice course, they receive credits to watch the entire Handbook of MRI Technique course on-demand, whenever it suits them.
The first five lectures of the Handbook course are designed to form the perfect revision for the topics covered by the MRI in Practice course, many offer a different perspective, and there are new additional animated diagrams throughout. Participants tell us that they really help to cement some of the concepts into place. The other five lectures are absolutely indispensable for those who are new to the field and wish to get up to speed with clinical practice in MRI. The course covers all of the most commonly-scanned body areas. These include the brain, spine, body, upper limb and lower limb.

Brand new for 2026 - 12 months FREE ACCESS to our amazing MRI Simulator.
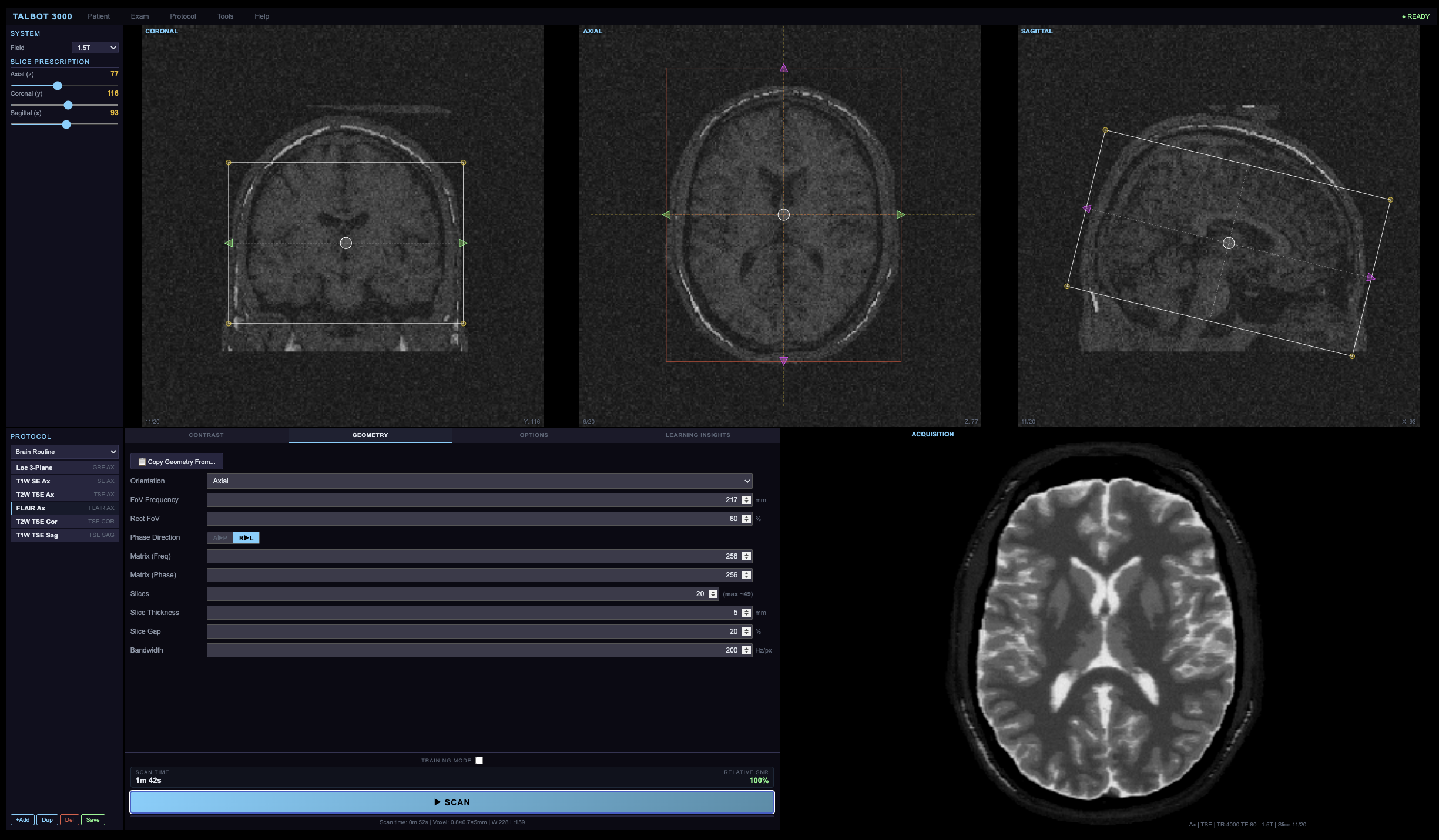
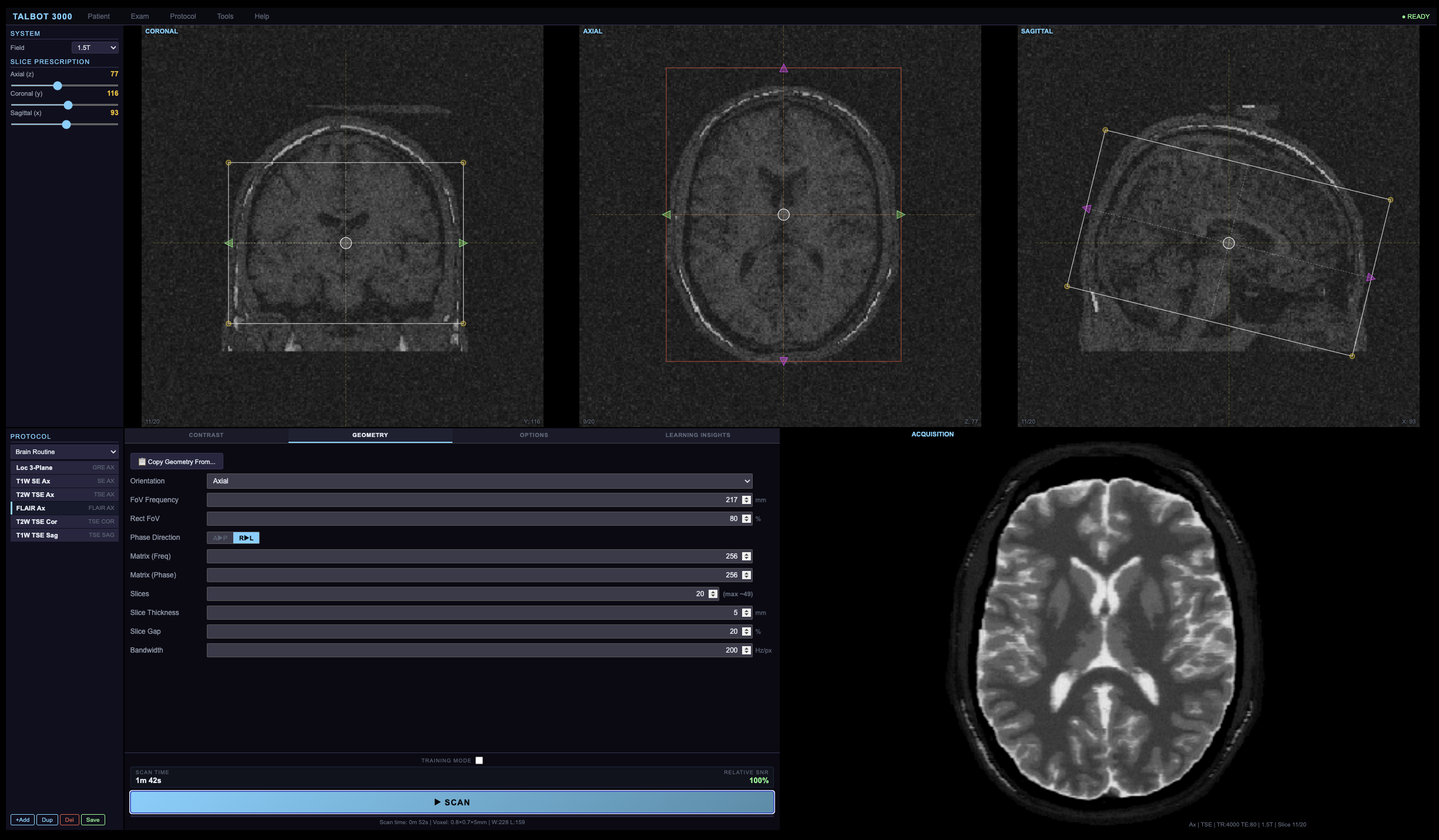
All of our lectures have used a simulated MRI scanner for the last 25 years. A photorealistic model and k-space simulator that we use when teaching Instrumentation and all the topics that ever relate physics to practice. To date the simulators were only used to create lecture materials - now participants can interact with the simulator just like a real scanner!
Magnetic resonance imaging is one of the most powerful diagnostic tools in modern medicine, yet the physics governing image contrast and image optimisation remains one of the most challenging topics for new practitioners to master. Understanding how pulse sequence parameters interact to produce clinically useful images requires more than textbook knowledge — it demands hands-on experience with the cause-and-effect relationships between acquisition settings and the resulting image.
Our new Virtual MRI Console addresses this educational challenge directly.
Developed by John Talbot, a learning specialist qualified to doctoral level in technology-enhanced learning, this is a browser-based simulator that places a functional MRI console in the hands of every student. No scanner access required. No patient risk. No booking conflicts. Just immediate, interactive, consequence-free exploration of MRI physics and image optimisation.
This simulator is dedicated to learning about image contrast and image optimisation and has been designed and built from the ground up so it meshes perfectly with our lectures. We include over 50 learning activities to perform using the simulator that relate directly to the lectures. Every topic we cover on the course relating to image contrast, artefacts and image optimisation can now be accurately explored using the simulator - remember, our name is MRI in PRACTICE and this simulator keeps us right at the forefront of that underpinning principle. No other course can match our perfect synchronicity between underpinning physics, our lectures, our book and your clinical outcomes.

The Educational Challenge
Newly qualified radiographers and trainee radiologists face a steep learning curve when they begin clinical MRI practice. The relationships between TR, TE, TI, flip angle, bandwidth, matrix size, field of view, and the resulting image contrast are complex, interdependent, and often counter-intuitive. Traditional teaching methods — lectures, textbooks, observation — can describe these relationships, but they cannot replicate the experience of sitting at a console and watching an image change in real time as each parameter is adjusted.
Scanner time is expensive, clinically allocated, and rarely available for teaching purposes. Even when training slots can be arranged, the learning opportunity is limited by the need to work with real patients and the pressure to produce clinically acceptable images. There is no opportunity to set deliberately poor parameters, observe the result, and understand why it failed.
Our simulator removes these barriers entirely.
Physics-Driven Simulation
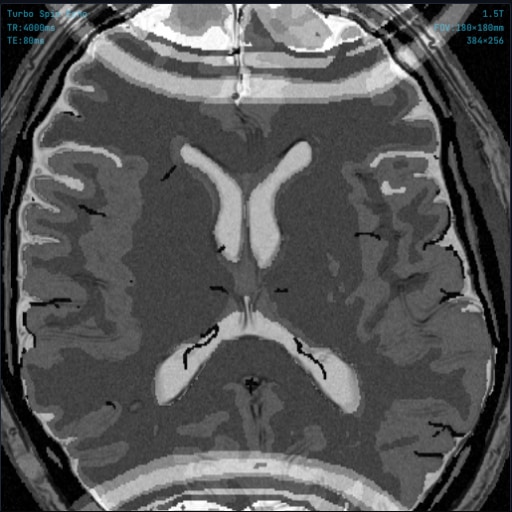
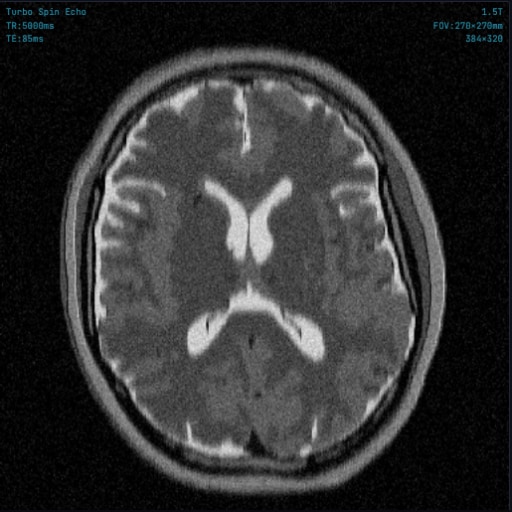
Unlike simplified teaching aids that display pre-rendered images or use look-up tables, our simulator calculates every pixel of every image from first principles using the Bloch equations. Signal intensity for each tissue type is computed in real time based on its T1, T2, and proton density values at the selected field strength, using the exact signal equations for the chosen pulse sequence. The result is a realistic synthetic MR image that responds to parameter changes with the same physics that governs a real scanner.
This approach means there are no artificial limits on what the student can explore. Every combination of parameters produces a physically meaningful result, even if that result is a poor image. A student who sets TR too short for T2 weighting will see the T1 contrast leak into their image. A student who selects an inappropriately high echo train length will see phase-direction blurring develop. A student who reduces bandwidth too aggressively will observe chemical shift artefact grow at fat–water interfaces. Every mistake becomes a teaching moment.
Capabilities
Pulse Sequence Library
The simulator provides a comprehensive library of pulse sequence implementations, each with correct signal equations, clinically appropriate parameter ranges, and generic protocol naming:
• Spin Echo (SE) — the foundational sequence for understanding T1, T2, and proton density weighting through TR and TE manipulation.
• Turbo Spin Echo (TSE) — with echo train length control, phase-direction blurring simulation, and magnetisation transfer contrast effects that realistically reduce grey–white matter differentiation at high ETL. ETL auto-sets to appropriate values based on matrix size.
• Gradient Echo (GRE) — implemented as three distinct sub-types: Spoiled (SPGR/FLASH/T1-FFE), Rewound (GRASS/FISP/FFE), and Balanced SSFP (TrueFISP/FIESTA/b-FFE), each with its own steady-state signal equation and characteristic contrast behaviour. Flip angle control demonstrates the Ernst angle relationship and its effect on T1 contrast.
• Inversion Recovery (IR) — with adjustable TI for selective tissue nulling. Presets automatically calculate field-strength-appropriate null points for white matter and grey matter.
• STIR — with field-strength-adaptive fat nulling and educational warnings about contraindication with gadolinium contrast.
• FLAIR — with field-strength-adaptive CSF nulling for periventricular lesion conspicuity.
• Single-Shot TSE (SS-TSE) — also known as HASTE (Siemens), SS-FSE (GE), or SSH-TSE (Philips). Fills the entire k-space in a single TR using very long echo trains, demonstrating the trade-off between acquisition speed and T2 blurring. ETL automatically matches the phase matrix size.
• Spin Echo EPI (SE-EPI) — single-shot echo planar imaging with spin echo preparation, demonstrating the extreme speed and characteristic geometric distortion, susceptibility artefacts, and chemical shift effects of EPI readouts.
• Gradient Echo EPI (GRE-EPI) — single-shot EPI with gradient echo preparation and T2* weighting, showing the increased susceptibility sensitivity compared to the spin echo variant.
• Diffusion Weighted Imaging (DWI) — based on the Stejskal-Tanner pulsed gradient scheme with adjustable b-value. Demonstrates how increasing diffusion sensitisation suppresses signal from freely mobile water while retaining signal from restricted diffusion environments. Generates b=0 reference images alongside diffusion-weighted images for comparison.
• Dixon (Two-Point) — acquires in-phase and opposed-phase echoes to generate separate water-only and fat-only images, plus the conventional in-phase and opposed-phase contrast. Demonstrates the chemical shift-based fat-water separation principle and the India ink artefact at fat-water boundaries.
Comprehensive Parameter Control
Every clinically relevant acquisition parameter is independently adjustable, giving students full control over the signal-to-noise, spatial resolution, and scan time trade-offs that define real-world protocol optimisation:
- Timing parameters: TR (2–10,000 ms), TE (1–300 ms), TI (10–5,000 ms), flip angle (1–90°), echo train length (2–32).
- Spatial parameters: FOV (100–500 mm), rectangular FOV (50–100%), phase encoding direction, frequency matrix (64–512), phase matrix (64–512), slice thickness (1–10 mm).
- Signal quality: NEX (1–4), parallel imaging acceleration (R = 1–4) with g-factor noise penalty, receiver bandwidth (50–500 Hz/pixel).
- Clinical options: frequency-selective fat saturation, intravenous gadolinium contrast simulation with flow void modelling, no phase wrap oversampling.
Multi-Anatomy, Multi-Field-Strength Design
The simulator includes accurately segmented tissue maps for two anatomical regions — axial brain (eight tissue types including cortical bone, CSF, grey matter, white matter, fat, muscle, skin, and blood) and sagittal knee (nine tissue types including articular cartilage, synovial fluid, ligament, cortical bone, and trabecular bone marrow). Each anatomy can be imaged at 0.5T, 1.5T, or 3.0T, with a complete tissue relaxation database providing field-strength-dependent T1, T2, and proton density values derived from the published topic literature.
More anatomical areas are scheduled to be added shortly - and all upgrades will be accessible to our participants over the duration of their access period.
Artefact Simulation
Understanding artefacts is essential for clinical practice, yet difficult to teach without hands-on experience. Our simulator reproduces all of the major acquisition-related artefacts encountered in routine imaging, each with physically correct behaviour that responds to parameter changes exactly as it would on a real scanner:
• Phase wrap-around — visible when the phase FOV is smaller than the anatomy, with correct wrap direction that follows the user's chosen phase-encoding axis. Removable with the no-phase-wrap oversampling toggle, which doubles acquisition in the phase direction at the cost of scan time.
• Chemical shift (Type 1) — bandwidth-dependent spatial misregistration at fat–water interfaces, correctly scaled to field strength and displayed in the frequency-encoding direction. Students can directly observe how increasing receiver bandwidth reduces the displacement at the expense of signal-to-noise ratio.
• Chemical shift (Type 2 / India ink) — signal cancellation at fat–water boundaries on opposed-phase gradient echo images, visible in the Dixon opposed-phase reconstruction and at specific echo times on GRE sequences.
• TSE blurring — T2-dependent signal decay across the echo train causing high-spatial-frequency attenuation in the phase-encoding direction. Becomes progressively more pronounced as echo train length increases, particularly visible on tissues with short T2.
• Truncation (Gibbs ringing) — oscillatory signal ringing at high-contrast interfaces caused by truncation of k-space at low matrix sizes. Correctly manifests as alternating bright and dark bands parallel to sharp tissue boundaries and diminishes as matrix resolution increases.
• Motion artefact — periodic ghosting propagated in the phase-encoding direction from simulated patient motion during acquisition. Demonstrates why motion ghosts appear along the phase axis regardless of the actual direction of movement.
• RF noise spike (zipper artefact) — simulates the effect of a corrupted data point in k-space from external RF interference, producing a characteristic striped zipper pattern across the image. Students can visualise the corresponding spike in the k-space display.
• Phase mismapping — k-space visualisation showing how data collected at different echo times during a TSE echo train maps to different phase-encoding lines, with an interactive graphic illustrating the relationship between echo position, k-space location, and resulting image contrast.
• EPI geometric distortion — susceptibility-induced spatial distortion characteristic of echo planar imaging sequences, demonstrating why EPI images show warping in the phase-encoding direction near air–tissue interfaces.
• Realistic noise modelling — signal-dependent Gaussian noise that responds correctly to voxel volume, number of signal averages (NEX/NSA), receiver bandwidth, field strength, and parallel imaging acceleration factor. Students can directly observe the SNR trade-offs inherent in every parameter change.
Aliasing

Chemical Shift
Echo Train Blur
Truncation
Our course covers 26 different artefacts - it's better that our new course participants can learn about these disasters on the simulator rather than on real patients during a busy list!
Protocol Optimisation Engine
The Optimise engine embedded within the simulator encapsulates the protocol design expertise that typically takes years of clinical experience to develop. For any given combination of pulse sequence, image weighting, anatomy, and field strength, the engine calculates a complete optimised protocol that balances diagnostic image quality against acquisition time — the fundamental trade-off at the heart of every MRI examination.
The optimisation considers the full parameter space: timing parameters for contrast, spatial parameters for resolution and coverage, receiver bandwidth for SNR and chemical shift control, parallel imaging for scan time reduction with appropriate g-factor trade-off, signal averaging for thin-slice SNR compensation, phase encoding direction for anatomy-appropriate wrap avoidance, and fat saturation where clinically indicated.
When the student engages with the built-in Learning Mode function, they can build a sequence/protocol from scratch - test the image appearance with every change and when they are done, the feedback report provides specific, educational commentary on every parameter that differs from the optimised protocol. This commentary explains not just what should change, but why — linking each adjustment to its physical consequence in terms of contrast, resolution, SNR, artefact behaviour, or scan time. Estimated scan times are displayed for both protocols, quantifying the time penalty of suboptimal parameter choices.
Technical Specification
Our simulator was designed an built in-house by Dr John Talbot, whose doctoral thesis was in the field of technology enhanced learning. It is delivered as a browser-based application requiring no software installation, plug-ins, or dedicated hardware. It runs in any modern web browser on desktop, laptop, or tablet devices. Image rendering is performed client-side in real time, providing instantaneous visual feedback as parameters are adjusted. The tissue maps, relaxation database, and edge detail overlays are served from a secure, authenticated server environment integrated with the MRI in Practice online learning platform.
Physics fans only…
SIGNAL MODEL
The Talbot 3000 computes signal intensity per voxel from the Bloch equations using tissue-specific T₁, T₂, and ρ values drawn from a field-strength-indexed relaxation database (0.5 T, 1.5 T, 3.0 T) compiled from Stanisz et al. (2005), de Bazelaire et al. (2004), and Gold et al. (2004). Six pulse sequences are implemented with closed-form steady-state signal equations: SE (ρ(1−e⁻ᵀᴿ/ᵀ¹)e⁻ᵀᴱ/ᵀ²), TSE with effective-TE echo-train modulation and MT attenuation coefficients, three GRE sub-types (spoiled: Ernst-angle steady-state; rewound: √(T₂/T₁)-dependent SSFP−FID; balanced: T₂/T₁-weighted bSSFP with near-unity ρ weighting), IR, STIR, and FLAIR with full longitudinal recovery/inversion terms. Fat saturation applies a 90% signal attenuation factor to lipid-labelled voxels. Gadolinium contrast modifies T₁ via the relaxivity relation 1/T₁,post = 1/T₁,pre + r₁[Gd], with r₁ = 4.5 mM⁻¹s⁻¹ at 1.5 T, and models flow-void signal loss in vascular structures.
K-SPACE RECONSTRUCTION PIPELINE
Image formation follows a physically authentic reconstruction chain. A 512×512 complex signal matrix S(x,y) is generated from the tissue map and Bloch-equation signal values, with separate fat and non-fat channels to permit frequency-direction chemical shift displacement (Δx = δf_cs/BW, where δf_cs = 224 Hz × B₀/1.5). The composite image undergoes a 2D radix-2 Cooley–Tukey FFT to produce complex k-space data K(kₓ,kᵧ). All subsequent manipulations occur in the frequency domain:
Matrix truncation. K-space is zeroed outside the user-selected frequency and phase acquisition window (m_freq × m_phase lines centred at DC). The resulting Sinc-convolution in image space produces Gibbs truncation ringing at sharp signal boundaries — the artefact is not simulated; it emerges naturally from the mathematics of finite Fourier sampling.
TSE T₂ modulation. For turbo spin echo acquisitions, each phase-encode line is weighted by exp(−ΔTE(k)/T₂,eff), where ΔTE(k) is the temporal offset from the effective TE based on the line's radial distance from k-space centre and the echo spacing (≈10 ms). This applies a low-pass filter in the phase direction whose width is proportional to ETL, reproducing the characteristic high-spatial-frequency attenuation responsible for TSE blurring.
Parallel imaging. At acceleration factor R > 1, every Rᵗʰ phase-encode line is zeroed in k-space, producing the FOV/R aliased reconstruction visible when GRAPPA reconstruction is disabled. Toggling GRAPPA ON restores fully-sampled k-space with an SNR penalty of √R × g, where the geometry factor g = 1 + 0.15(R−1) models spatially-varying noise amplification from coil sensitivity inversion.
Noise injection. Complex Gaussian noise is added to k-space prior to inverse transform: n(k) ~ ℂ𝒩(0, σₖ²), where σₖ is derived from the voxel-volume SNR model σ ∝ V_vox½ × √NEX × B₀ / (√BW × √R × g). This is physically correct: receiver noise enters in the frequency domain, producing spatially uncorrelated noise after magnitude reconstruction.
K-space spike artefacts. User-placed point impulses are inserted at (kₓ,kᵧ) with Hermitian-conjugate symmetry enforced at (−kₓ,−kᵧ) to maintain real-valued image reconstruction. Each spike produces a sinusoidal modulation pattern across the image at a spatial frequency and orientation determined by its k-space coordinates — reproducing the 'corduroy' or 'zipper' artefact caused by RF interference or electronic faults.
The manipulated k-space undergoes inverse 2D FFT followed by magnitude reconstruction |√(Re² + Im²)|. The result is downsampled to the acquisition matrix, with optional zero-fill interpolation (k-space zero-padding) for display. Window/level adjustment and a transparent anatomical edge overlay (Sobel gradient magnitude extracted from original MR data) are applied as final compositing steps.
ARTEFACT FIDELITY
Every artefact in the Talbot 3000 is a consequence of the acquisition physics, not a post-hoc visual effect. Gibbs ringing arises from k-space truncation. Phase wrap arises from sub-Nyquist spatial sampling. Chemical shift arises from the fat–water frequency offset in the readout gradient. TSE blurring arises from T₂ decay across the echo train. Parallel imaging aliasing arises from phase-encode undersampling. Noise texture arises from complex Gaussian contamination in the frequency domain. The simulator does not contain a single line of code that draws, overlays, or fakes an artefact. They emerge.
What exactly is included in the price?
In summary, participants will enjoy:
✔️ 4 days online teaching via our custom-built online learning environment
✔️ All-day access to the world-renowned MRI educators Dr. Catherine Westbrook and Dr. John Talbot via messages, chat, text, audio and video channels.
✔️ 26 streaming lectures featuring our famous computer generated imagery, namely…
✔️ 16 MRI in Practice lectures (20 hours)
✔️ 12-month access to our 10 Handbook of MRI lectures (6 hours of revision videos and clinical technique instruction).
✔️ 12-month access to our incredible MRI Simulator.
✔️ Over 50 valuable learning exercises to run on our simulator that link theory to practice.
✔️ Interactive revision sessions for every main topic.
✔️ 100 interactive animations accessed from our learning portal.
All at a price that beats any of our competitors. In addition, the course is a valuable source of CPD:
- UK - Society and College of Radiographers fulfilling learning outcomes 1,2,3,6,7,9,11,19 as defined by CPD Now.
- Australia - ASMIRT - offers 30 HOURS of CPD appellation
Your assurance of quality
If you are a manager or practice education lead, the price is important, but you will also be looking for the highest quality educational experience for your staff. The quality of this course is assured:
- We are not only endorsed by the Society and College of Radiographers, but also by over 20 international professional bodies and educational establishments.
- We are the go-to MRI education provider for the NHS and several of the largest private medical companies.
- Our courses have been used to enhance the MRI curriculum in university programmes in Chicago, Cambridge, Oxford, Dublin, Columbia (Missouri), Qatar, Sharjah, and Zagreb.
- The course has also been adopted by professional bodies in Australia, Sweden, Norway, Croatia, Kuwait, Malta, Romania, Kenya and Serbia.
- The presenters, Dr Catherine Westbrook and Dr John Talbot are both industry-recognised experts in online learning (since 2005) both hold Master of Science Degrees in MRI, are both qualified in Education to Doctoral level and are both Fellows of the Higher Education Academy.
We are not aware of any other MRI courses having a faculty qualified to this level. It seems obvious that an MRI education course should use presenters who are qualified in both MRI and education, but not all of them are. Please take care when deciding on a course provider, fraudulent or fake education is becoming an increasing concern in pedagogical circles, especially with recent developments in AI. If you are in any doubt about an education provider not having the necessary qualifications to be providing educational services, ask to see the learning and teaching certification for all members of their faculty. This must at least be a PgC in Learning and Teaching, and for teaching post graduates (such as radiographers) it should be an EdD or equivalent.
Our course currently enjoys an average customer excellence rating of [newfeedback-D10]% from our [newfeedback-D11] respondents attending between [newfeedback-D12] and [newfeedback-D13]. These statistics are collected anonymously at the end of every course via Google Forms.
Our current global participant ratings are shown below...
Our Forthcoming Courses
Our Forthcoming Courses
Western Hemisphere
MRI in Practice Online
MRI in Practice Online
A little taster of what we offer on our online course...
The online course uses a combination of HD streaming video to present our trademark CGI graphics and user-friendly analogies that give our course an unsurpassed conceptual clarity that our participants really love. Our lectures use computer-generated imagery produced in-house and are the result of 15 years development and over 1000 CGI models and animations.
Some online course providers present their lectures directly from Zoom or by screen-sharing their own computer - this tends to result in a sub-optimal, jerky, low-resolution presentation with occasional dropouts due to loss of internet connection by the host and having to share bandwidth between a number of participants.
We don't do this, as teaching experts with over 30 years of experience in distance learning and blended learning (and, with formal academic qualifications in technology-enhanced learning) we use a blend of live face-to-face live sessions in Zoom (to introduce and conclude the course), an instant messaging and VoIP social platform which allows ad hoc Q/A and streaming HD video that is delivered via a professional broadcast server (AWS) to ensure the very highest quality and uninterrupted service , here is an example of what you can expect from our lectures…
Please feel free to share this video with anyone you think might be interested. There is a share icon at the top right corner of the screen when you hover your cursor over the window.